Hypertension Requiring Continuous Infusion of Intravenous Antihypertensives
Abstract
Background
Acute blood pressure (BP) management in neurologic patients is paramount. Different neurologic emergencies dictate various BP goals. There remains a lack of literature determining the optimal BP regimen regarding safety and efficacy. The objective of this study was to identify which intravenous antihypertensive is the most effective and safest for acute BP management in neurologic emergencies.
Methods
Ovid EBM (Evidence Based Medicine) Reviews, Ovid Embase, Ovid Medline, Scopus, and Web of Science Core Collection were searched from inception to August 2020. Randomized controlled trials or comparative observational studies that evaluated clevidipine, nicardipine, labetalol, esmolol, or nitroprusside for acute neurologic emergencies were included. Outcomes of interest included mortality, functional outcome, BP variability, time to goal BP, time within goal BP, incidence of hypotension, and need for rescue antihypertensives. The Grading of Recommendations Assessment, Development, and Evaluation approach was used to evaluate the degree of certainty in the evidence available.
Results
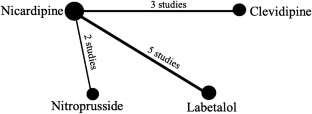
A total of 3878 titles and abstracts were screened, and 183 articles were selected for full-text review. Ten studies met the inclusion criteria; however, the significant heterogeneity and very low quality of studies precluded a meta-analysis. All studies included nicardipine. Five studies compared nicardipine with labetalol, three studies compared nicardipine with clevidipine, and two studies compared nicardipine with nitroprusside. Compared with labetalol, nicardipine appears to reach goal BP faster, have less BP variability, and need less rescue antihypertensives. Compared with clevidipine, nicardipine appears to reach goal BP goal slower. Lastly, nicardipine appears to be similar for BP-related outcomes when compared with nitroprusside; however, nitroprusside may be associated with increased mortality. The confidence in the evidence available for all the outcomes was deemed very low.
Conclusions
Because of the very low quality of evidence, an optimal BP agent for the treatment of patients with neurologic emergencies was unable to be determined. Future randomized controlled trials are needed to compare the most promising agents.
Access options
Buy single article
Instant access to the full article PDF.
39,95 €
Price includes VAT (Indonesia)
References
-
Ohwaki K, Yano E, Nagashima H, Hirata M, Nakagomi T, Tamura A. Blood pressure management in acute intracerebral hemorrhage: Relationship between elevated blood pressure and hematoma enlargement. Stroke. 2004;35(6):1364–7.
-
Moullaali TJ, Wang X, Martin RH, et al. Blood pressure control and clinical outcomes in acute intracerebral haemorrhage: a preplanned pooled analysis of individual participant data. Lancet Neurol. 2019;18(9):857–64.
-
Kuramatsu JB, Gerner ST, Schellinger PD, et al. Anticoagulant reversal, blood pressure levels, and anticoagulant resumption in patients with anticoagulation-related intracerebral hemorrhage. JAMA J Am Med Assoc. 2015;313(8):824–36.
-
Aronson S, Dyke CM, Stierer KA, et al. The ECLIPSE trials: Comparative studies of clevidipine to nitroglycerin, sodium nitroprusside, and nicardipine for acute hypertension treatment in cardiac surgery patients. Anesth Analg. 2008;107(4):1110–21.
-
Varelas PN, Abdelhak T, Corry JJ, et al. Clevidipine for acute hypertension in patients with subarachnoid hemorrhage: a pilot study. Int J Neurosci. 2014;124(3):192–8.
-
Ndefo UA, Erowele GI, Ebiasah R, Green W. Clevidipine: a new intravenous option for the management of acute hypertension. Am J Heal Pharm. 2010;67(5):351–60.
-
Graffagnino C, Bergese S, Love J, et al. Clevidipine rapidly and safely reduces blood pressure in acute intracerebral hemorrhage: the ACCELERATE trial. Cerebrovasc Dis. 2013;36(3):173–80.
-
Page MJ, McKenzie JE, Bossuyt PM, The PRISMA, et al. Statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372.
-
Rohatgi A. WebPlotDigitizer Version 4.4. [Internet]. 2020 [cited 2021 Jun 15]. https://automeris.io/WebPlotDigitizer.
-
Sterne JAC, Savović J, Page MJ, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:1–8.
-
Wells G, Shea B, O'Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Internet]. 2020. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
-
MedCalc Software Ltd. Relative risk calculator. Version 20.009 [Internet]. [cited 2021 Jul 20]. https://www.medcalc.org/calc/relative_risk.php
-
Murad MH, Mustafa RA, Schünemann HJ, Sultan S, Santesso N. Rating the certainty in evidence in the absence of a single estimate of effect. Evid Based Med. 2017;22(3):85–7.
-
Hecht JP, Richards PG. Continuous-infusion labetalol vs nicardipine for hypertension management in stroke patients. J Stroke Cerebrovasc Dis. 2018;27(2):460–5.
-
Liu-Deryke X, Levy PD, Parker D, Coplin W, Rhoney DH. A prospective evaluation of labetalol versus nicardipine for blood pressure management in patients with acute stroke. Neurocrit Care. 2013;19(1):41–7.
-
Ortega-Gutierrez S, Thomas J, Reccius A, et al. Effectiveness and safety of nicardipine and labetalol infusion for blood pressure management in patients with intracerebral and subarachnoid hemorrhage. Neurocrit Care. 2013;18(1):13–9.
-
Allison TA, Bowman S, Gulbis B, Hartman H, Schepcoff S, Lee K. Comparison of clevidipine and nicardipine for acute blood pressure reduction in patients with stroke. J Intensive Care Med. 2019;34(11–12):990–5.
-
Finger JR, Kurczewski LM, Brophy GM. Clevidipine versus nicardipine for acute blood pressure reduction in a neuroscience intensive care population. Neurocrit Care. 2017;26(2):167–73.
-
Rosenfeldt Z, Conklen K, Jones B, Ferrill D, Deshpande M, Siddiqui FM. Comparison of nicardipine with clevidipine in the management of hypertension in acute cerebrovascular diseases. J Stroke Cerebrovasc Dis. 2018;27(8):2067–73.
-
Roitberg BZ, Hardman J, Urbaniak K, et al. Prospective randomized comparison of safety and efficacy of nicardipine and nitroprusside drip for control of hypertension in the neurosurgical intensive care unit. Neurosurgery. 2008;63:115–21.
-
Suri MFK, Vazquez G, Ezzeddine MA, Qureshi AI. A multicenter comparison of outcomes associated with intravenous nitroprusside and nicardipine treatment among patients with intracerebral hemorrhage. Neurocrit Care. 2009;11(1):50–5.
-
Woloszyn AV, McAllen KJ, Figueroa BE, DeShane RS, Barletta JF. Retrospective evaluation of nicardipine versus labetalol for blood pressure control in aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2012;16(3):376–80.
-
Liu-DeRyke X, Janisse J, Coplin WM, Parker D, Norris G, Rhoney DH. A comparison of nicardipine and labetalol for acute hypertension management following stroke. Neurocrit Care. 2008;9(2):167–76.
-
Chung PW, Kim JT, Sanossian N, et al. Association between hyperacute stage blood pressure variability and outcome In patients with spontaneous intracerebral hemorrhage. Stroke. 2018;49(2):348–54.
-
Divani AA, Liu X, Di Napoli M, et al. Blood pressure variability predicts poor in-hospital outcome in spontaneous intracerebral hemorrhage. Stroke. 2019;50(8):2023–9.
-
Mistry EA, Mehta T, Mistry A, et al. Blood pressure variability and neurologic outcome after endovascular thrombectomy: a secondary analysis of the BEST study. Stroke. 2020;51:511–8.
-
Kim TJ, Park HK, Kim JM, et al. Blood pressure variability and hemorrhagic transformation in patients with successful recanalization after endovascular recanalization therapy: a retrospective observational study. Ann Neurol. 2019;85(4):574–81.
-
Ascanio LC, Enriquez-Marulanda A, Maragkos GA, et al. Effect of blood pressure variability during the acute period of subarachnoid hemorrhage on functional outcomes. Neurosurgery. 2020;87(4):779–87.
-
Poyant JO, Kuper PJ, Mara KC, et al. Nicardipine reduces blood pressure variability after spontaneous intracerebral hemorrhage. Neurocrit Care. 2019;30(1):118–25.
-
Peacock WF, Varon J, Baumann BM, et al. CLUE: A randomized comparative effectiveness trial of IV nicardipine versus labetalol uwse in the emergency department. Crit Care. 2011;15(3):R157.
-
Erickson AL, DeGrado JR, Fanikos JR. Clevidipine: a short-acting intravenous dihydropyridine calcium channel blocker for the management of hypertension. Pharmacotherapy. 2010;30(5):515–28.
-
Rose JC, Mayer SA. Optimizing blood pressure in neurological emergencies. Neurocrit Care. 2004;1(3):287–99.
-
Turndorf H, Ransohoff J. Intraeranial pressure changes induced by sodium nitroprusside in patients with intracranial mass lesions. J Neurosurg. 1978;48:329–31.
-
Appiah KO, Nath M, Manning L, et al. Increasing blood pressure variability predicts poor functional outcome following acute stroke. J Stroke Cerebrovasc Dis. 2021;30(1):105466.
-
Clevidipine [Package insert]. Cary, NC: Chiesi USA, Inc. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/022156s007lbl.pdf.
-
Nitroprusside [Package insert]. Lenoir, NC: Exela Pharma Sciences, LLC. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/209387s000lbl.pdf.
-
Labetalol [Package insert]. San Diego, CA: Prometheus Laboratories Inc. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/018716s026lbl.pdf.
-
Nicardipine [Package insert]. Shirley, NY: American Regent, Inc. Available at: https://americanregent.com/media/2888/nicardipine_pi-insert_rev-mar2020_21apr2020.pdf.
Funding
This study was partially funded by the Mayo Midwest Pharmacy Research Committee.
Author information
Authors and Affiliations
Contributions
C.S.B., L.O.J.S., A.E.M., D.C., and A.A.R. designed the study. C.S.B, A.E.M, K.F, L.O.J.S, and D.G. collected data, and C.S.B, A.E.M, L.O.J.S, D.C, and A.A.R analyzed and interpreted the data. C.S.B, L.O.J.S, A.E.M, and K.F drafted the article and all authors revised and approved of the final version. Previously presented in part at the 2021 American College of Clinical Pharmacy Annual Meeting.
Corresponding author
Ethics declarations
Conflicts of interest
D.C.: Intellectual property royalties from Diagnostic Robotics, Israel. Intellectual property royalties from Osler Diagnostics, UK. A.A.R: Received royalties from Oxford, Elsevier, and Springer. Served on advisory board for Astra Zeneca and Novo Nordisk. Served on adverse event adjudication committee for Boston Scientific. The remaining authors have no conflicts to disclose.
Ethical approval/informed consent
Given this is a systematic review, no institutional review board approval was required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Brown, C.S., Oliveira J. e Silva, L., Mattson, A.E. et al. Comparison of Intravenous Antihypertensives on Blood Pressure Control in Acute Neurovascular Emergencies: A Systematic Review. Neurocrit Care 37, 435–446 (2022). https://doi.org/10.1007/s12028-021-01417-8
-
Received:
-
Accepted:
-
Published:
-
Issue Date:
-
DOI : https://doi.org/10.1007/s12028-021-01417-8
Keywords
- Antihypertensives
- Blood pressure
- Acute stroke
- Subarachnoid hemorrhages
- Brain hemorrhage
Source: https://link.springer.com/article/10.1007/s12028-021-01417-8
0 Response to "Hypertension Requiring Continuous Infusion of Intravenous Antihypertensives"
Post a Comment